
Skull Base Surgery In Hyderabad
Skull base surgery represents one of the most technically demanding subspecialties in neurosurgery, addressing complex pathologies located at the junction between the brain and skull. The skull base contains vital neurovascular structures including cranial nerves, major blood vessels, and critical brain regions packed into a confined anatomical space. Tumours, vascular lesions, infections, and congenital abnormalities in this area require highly specialised surgical expertise and advanced techniques.
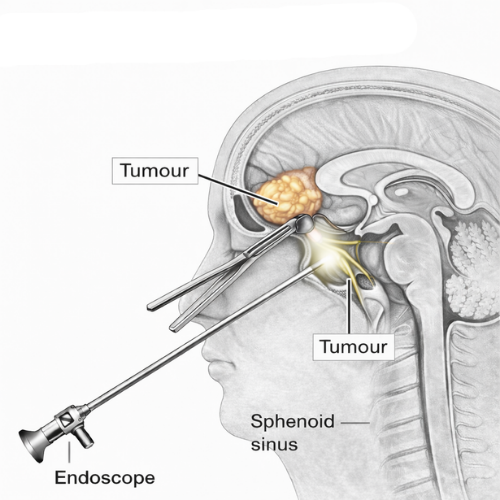
Modern skull base surgery has evolved dramatically with the development of minimally invasive endoscopic approaches, advanced microsurgical techniques, and sophisticated imaging technology. These innovations allow neurosurgeons to access previously unreachable areas through smaller openings, resulting in reduced brain manipulation, faster recovery, and improved outcomes. Surgery in this region demands meticulous anatomical knowledge, refined surgical skills, and careful planning to preserve neurological function while achieving treatment goals.

“Skull base surgery is where anatomy, technology, and surgical precision converge. Success requires not just removing the pathology, but protecting every critical structure in this densely packed region.”
Dr. Sai Shiva Tadakamalla, Brain & Spine Surgeon
Skull base surgery is performed by Dr. Sai Shiva Tadakamalla, a fellowship trained skull base neurosurgeon in Hyderabad, utilising both endoscopic and open microsurgical approaches with focus on neurological preservation, cosmetic outcomes, and evidence based care tailored to individual patient needs.
What Is Skull Base Surgery?
Skull base surgery encompasses surgical procedures performed on tumours, vascular abnormalities, and other pathologies located at the bottom surface of the skull. This anatomical region is divided into anterior, middle, and posterior compartments, each containing different critical structures. The anterior skull base sits behind the forehead and nose, the middle region includes the area around the pituitary gland and cavernous sinus, while the posterior skull base extends toward the back of the head near the brainstem and cerebellum.
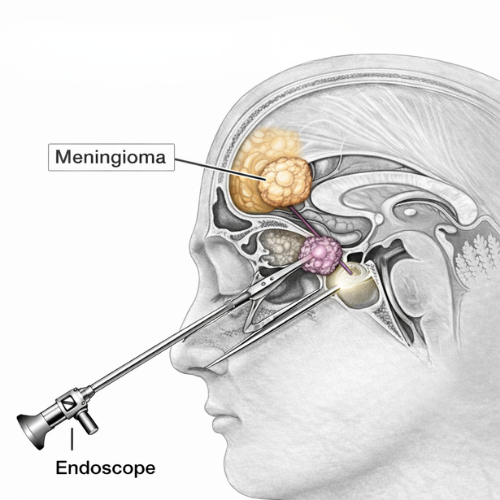
Surgical approaches are chosen based on lesion location, size, and relationship to surrounding structures. Endoscopic endonasal approaches access tumours through the nasal passages without external incisions. Traditional craniotomy approaches provide direct visualisation when needed. Some complex cases may require combined approaches or staged procedures. The primary objectives include complete or maximum safe resection, preservation of neurological function, and restoration of skull base integrity.
Consult an experienced skull base neurosurgeon in Hyderabad for comprehensive evaluation of complex skull base pathologies.
Conditions Treated With Skull Base Surgery by Dr. Sai Shiva Tadakamalla
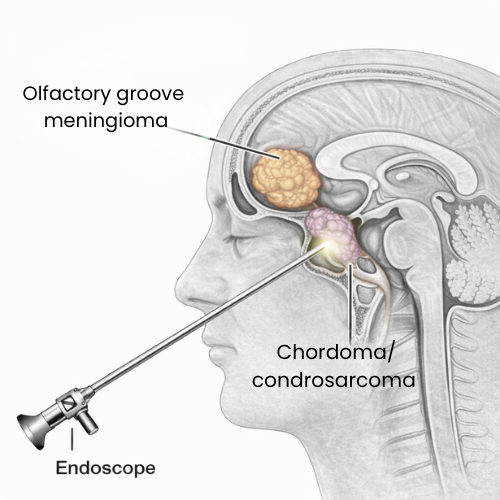
Anterior Skull Base Tumours
Surgical management of tumours located behind the forehead and nasal cavity including olfactory groove meningiomas, frontal sinus tumours, and ethmoid region pathologies. Advanced approaches allow tumour removal while preserving olfactory function and reconstructing skull base defects.
Posterior Skull Base Tumours
Treatment of lesions at the back of the skull including acoustic neuromas, jugular foramen tumours, foramen magnum meningiomas, and petroclival lesions. Surgery focuses on tumour removal while protecting cranial nerves controlling hearing, balance, swallowing, and facial movement.
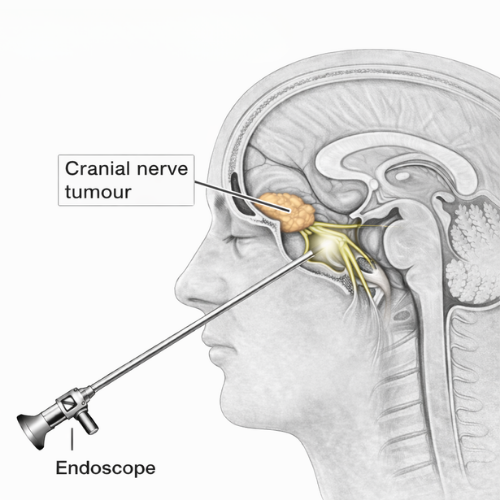
Cranial Nerve Tumours
Specialised removal of tumours arising from cranial nerves such as acoustic neuromas affecting hearing and balance nerves, trigeminal schwannomas, and other nerve sheath tumours. Emphasis on nerve preservation techniques and functional outcome optimisation.
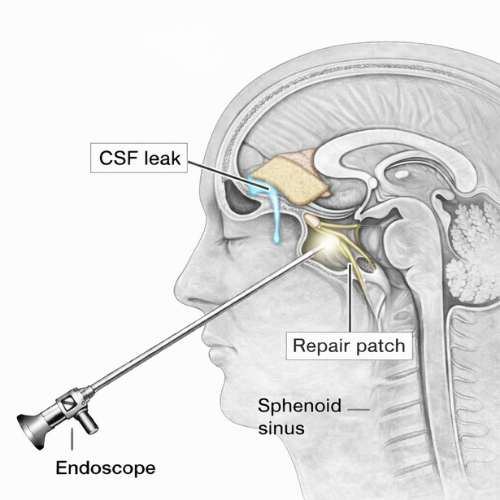
CSF Leak Repair
Surgical correction of cerebrospinal fluid leaks through skull base defects using endoscopic or open techniques. Treatment prevents meningitis risk, eliminates persistent nasal drainage, and restores normal skull base integrity with tissue grafts and reconstruction.
Endoscopic Skull Base Surgery
Minimally invasive approach accessing skull base pathologies through the nasal passages without external incisions. Provides excellent visualisation for midline tumours, pituitary lesions, clival pathologies, and CSF leak repairs with reduced recovery time and improved cosmetic outcomes.
Symptoms Of Skull Base Pathologies
Symptoms of skull base lesions depend on location and involvement of nearby structures. Common presentations include:
- Hearing loss, tinnitus, or balance disturbances
- Facial numbness, weakness, or pain
- Vision changes, double vision, or visual field defects
- Persistent headaches or facial pressure
- Nasal obstruction or recurrent sinus infections
- Clear fluid drainage from the nose (CSF leak)
- Swallowing or speech difficulties
- Hormonal imbalances from pituitary involvement
- Seizures or changes in consciousness
- Cranial nerve palsies affecting eye movement or facial sensation
Early consultation with a skull base specialist allows accurate diagnosis and optimal treatment planning for complex conditions.
When Is Skull Base Surgery Recommended?
Skull base surgery may be recommended in various clinical scenarios:
Symptomatic Lesions:
When tumours or abnormalities cause progressive neurological symptoms, hearing loss, vision changes, or facial nerve dysfunction, surgical intervention may prevent permanent deficits.
Progressive Growth:
Enlarging lesions on serial imaging scans, even if currently asymptomatic, may warrant treatment to prevent future complications and preserve neurological function.
Mass Effect:
Lesions causing compression of the brain, brainstem, or cranial nerves require decompression to relieve pressure and restore normal function.
Tissue Diagnosis:
When imaging cannot definitively characterise a lesion, surgical biopsy provides tissue for accurate diagnosis and treatment planning.
CSF Leaks:
Persistent cerebrospinal fluid leaks through skull base defects require surgical repair to prevent meningitis and restore normal anatomy.
Hemifacial Spasm or Trigeminal Neuralgia:
Debilitating facial pain or spasm refractory to medical management may benefit from microvascular decompression procedures.
Treatment decisions are individualised following comprehensive evaluation including advanced imaging, audiological testing when appropriate, ophthalmological assessment, and multidisciplinary discussion to optimise outcomes.
Surgical Approaches In Skull Base Surgery
- Endoscopic Endonasal Approach
A minimally invasive technique accessing the skull base through the nasal passages using advanced endoscopic equipment. This approach offers excellent visualisation of midline skull base pathologies including pituitary tumours, clival lesions, and sellar region abnormalities without external incisions or brain retraction.
- Retrosigmoid Approach
A posterior fossa approach used for acoustic neuromas and other cerebellopontine angle lesions. This technique provides access to the hearing and facial nerves with good preservation potential and direct visualisation of the brainstem.
- Pterional Approach
A versatile frontotemporal craniotomy allowing access to the anterior and middle skull base, cavernous sinus region, and upper basilar artery complex through a cosmetically hidden incision.
- Middle Fossa Approach
Used for small acoustic neuromas and superior petroclival lesions, this technique accesses the internal auditory canal from above with potential for hearing preservation in selected patients.
- Far Lateral Approach
An extended posterior approach for lesions at the foramen magnum and lower clivus, providing access to the cervicomedullary junction and vertebral artery region.
- Combined Approaches Complex lesions may require staged procedures or combination of multiple approaches to achieve safe and complete resection while minimising complications.
Recovery After Skull Base Surgery
Recovery following skull base surgery varies significantly based on approach, lesion location, and individual patient factors:
- Hospital Stay: Patients typically remain hospitalised for 3 to 7 days depending on the procedure complexity and neurological status. Some minimally invasive procedures may allow earlier discharge.
- Neurological Monitoring: Close observation of cranial nerve function, vision, hearing, and general neurological status is maintained during recovery. Some deficits may improve gradually over weeks to months.
- Pain Management: Headaches and discomfort are common initially but typically well controlled with appropriate medications. Endoscopic approaches generally involve less post operative pain.
- Activity Restrictions: Strenuous activities are avoided for several weeks. Specific restrictions depend on the surgical approach and may include limitations on nose blowing, heavy lifting, or straining.
- Rehabilitation: Some patients benefit from physical therapy, speech therapy, or vestibular rehabilitation depending on which functions were affected by the pathology or surgery.
- Follow Up Imaging: Regular MRI scans monitor for residual disease, recurrence, and healing. The frequency and duration of surveillance is determined by the specific pathology treated.
Why Choose Dr. Sai Shiva Tadakamalla For Skull Base Surgery?
Fellowship Trained Expertise
Completed advanced fellowship training in skull base surgery at a premier national institute, providing specialised expertise in complex pathologies.
Dual Technique Proficiency
Skilled in both modern endoscopic approaches and traditional microsurgical techniques, selecting the optimal approach for each patient.
Neurological Preservation Focus
Prioritises preservation of critical functions including vision, hearing, facial nerve, and hormonal balance through meticulous surgical technique.
Collaborative Care Model
Works with ENT surgeons, endocrinologists, ophthalmologists, and radiation oncologists to provide comprehensive multidisciplinary skull base care.

“Every skull base case is unique. Success comes from thorough planning, precise execution, and honest communication about realistic goals and potential outcomes.”
Dr. Sai Shiva Tadakamalla, Brain & Spine Surgeon in Hyderabad
Schedule a consultation with an experienced skull base neurosurgeon in Hyderabad to discuss personalised treatment options for complex skull base conditions.
FAQs
How long does skull base surgery take?
Surgery duration varies widely based on lesion complexity, location, and approach chosen, typically ranging from 3 to 8 hours or longer for extensive pathologies.
Will I lose my hearing after acoustic neuroma surgery?
Hearing preservation depends on tumour size, preoperative hearing level, and surgical approach. Smaller tumours with good baseline hearing have better preservation potential. Your surgeon will discuss realistic expectations based on your individual situation.
What are the main risks of skull base surgery?
Risks vary by location and may include CSF leak, meningitis, cranial nerve injury affecting hearing, vision, or facial movement, stroke, and bleeding. Modern techniques have significantly reduced these risks, and they are thoroughly discussed before surgery.
Is endoscopic skull base surgery safer than traditional approaches?
Each approach has specific advantages and limitations. Endoscopic techniques offer reduced brain manipulation and faster recovery for midline lesions, while traditional approaches may be necessary for lateral or complex tumours. The best approach depends on individual pathology.
How long is recovery after skull base surgery?
Recovery varies significantly. Some patients resume light activities within 2 to 3 weeks, while others may require several months for complete recovery, particularly when neurological deficits need time to improve.
Will I need radiation therapy after surgery?
Additional treatment depends on the pathology, extent of resection, and tumour behaviour. Some benign tumours require only surveillance, while others may benefit from adjuvant radiation. This is determined by pathology results and multidisciplinary discussion.
Can skull base tumours recur after surgery?
Recurrence risk depends on tumour type and completeness of removal. Benign lesions completely removed have low recurrence rates, while more aggressive tumours or those with incomplete resection may require ongoing monitoring and additional treatment.
